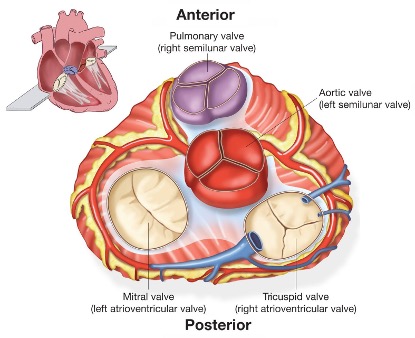
Transcatheter Valve Therapies - TAVR, TMVR, TTVR, TPVI
Transcatheter Aortic Valve Replacement (TAVR): A minimally invasive procedure used to replace a diseased aortic valve with a new valve, delivered through a catheter inserted into the blood vessels. TAVR is often performed on patients with severe aortic stenosis who are considered high-risk for traditional open-heart surgery.
Transcatheter Mitral Valve Replacement (TMVR): Similar to TAVR, TMVR involves replacing a malfunctioning mitral valve using a catheter-based approach. This procedure is typically considered for patients with mitral valve regurgitation who are not candidates for surgery.
Transcatheter Tricuspid Valve Replacement (TTVR): TTVR is a procedure aimed at replacing a damaged tricuspid valve through catheter-based delivery. It is performed to treat severe tricuspid valve disease, often in patients with significant comorbidities or previous surgeries.
Transcatheter Pulmonary Valve Implantation (TPVI): TPVI is a minimally invasive procedure used to replace a dysfunctional pulmonary valve. It is commonly performed in patients with congenital heart defects, such as Tetralogy of Fallot, who have undergone previous surgical repair and require valve replacement.
Aortic Stenosis and Transcatheter Aortic Valve Replacement (TAVR / TAVI)-
Aortic Stenosis and Transcatheter Aortic Valve Replacement (TAVR / TAVI)- The aortic valve is the most important of the four heart valves that control the flow of blood in and out of the heart. If the aortic valve becomes abnormally narrow (aortic stenosis) or leaks (aortic regurgitation), the heart must work harder to pump the same amount of blood. As a result, the heart muscle thickens, and the chambers of the heart may enlarge and ultimately lead to heart failure.
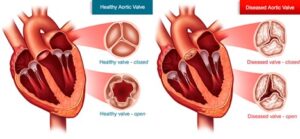
If aortic valve disease is left untreated, it leads to breathlessness, chest pain, blackouts, heart failure and eventually death.
In patients with severe aortic stenosis, the only effective long-term treatment is to replace the valve.
Transcatheter Aortic Valve Replacement (TAVR / TAVI)
Transcatheter aortic valve implantation (TAVI) or replacement (TAVR) is a minimally invasive procedure that involves inserting a catheter into a blood vessel in your upper leg and passing it towards your native aortic valve to implant a new valve.
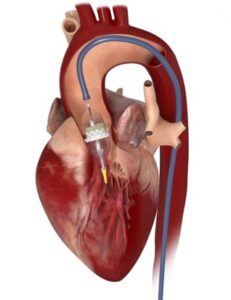
Under local anaesthetic, a small tube called a sheath will be inserted in the artery at the top of one of your legs or arm for taking pictures during the procedure. A slightly bigger sheath will be inserted into the artery at the top of your other leg, which the new valve will go through. Sometimes, a temporary pacemaker will be put into your heart through a vein in your neck or leg in case the doctor needs to speed up your heart during the procedure.
Catheters (small tubes) are passed through the bigger sheath to pass a long ‘guide wire’ across the narrowed aortic valve. The new aortic valve is then advanced over this wire (like a train on rail tracks) until it is in place inside your narrowed valve and then expanded to push the narrowed valve open, creating a new valve within it. A small balloon (‘balloon catheter’) may be used to widen your narrowed aortic valve before the new aortic valve is placed. It may also be used to widen the new aortic valve after it has been implanted.
It is a low risk minimally invasive procedure with quick recovery and short hospital stay.
The main advantages of this technique are that the heart doesn’t need to be stopped, so a heart-lung (bypass) machine doesn’t need to be used, and it avoids making a large cut (incision) in your chest. This puts less strain on the body and may mean TAVI is more suitable for people who are at high risk to have a conventional valve replacement or need a quick recovery with shorter hospital stay.
Mitral Trancatheter Edge to Edge Repair (M-TEER)
What is Mitral regurgitation?
The Mitral valve is located between the left atrium and the left ventricle and controls the flow of blood between these two heart chambers. Mitral regurgitation (MR) occurs when the Mitral valve does not close sufficiently, and consequently allows blood to flow backwards from the left ventricle into the left atrium. MR places substantial strain on the heart, as the heart must work harder to pump blood into the left ventricle, against the backflow of blood regurgitating through the Mitral valve.
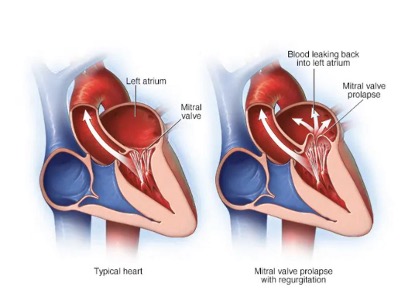
Mitral regurgitation can cause building up of fluid in the body, can lead to shortness of breath and tiredness or fatigue. Later stages, it can lead to atrial fibrillation (irregular heart rhythm, worsening of liver and kidney function.
Without treatment, Mitral regurgitation usually worsens with time. Although medicines can reduce the symptoms, the effects of long-term MR can result in symptoms and signs of heart failure (breathlessness, fatigue, fluid over-load) despite optimal medical treatment. In these cases, surgical intervention may be necessary to repair the leaking Mitral valve. Until recently, Mitral valve repair has involved open-heart surgery. This method requires a general anaesthetic, the breast bone to be cut, and open-heart surgery to be performed. An alternative, less invasive form of Mitral valve repair may now be offered, whereby the Mitral valve is repaired percutaneously (“through the skin”) via the groin using a transcatheter (thin flexible tube). This method does not require the breast bone to be cut or open-heart surgery to be performed. It is called a ‘Mitral Transcatheter Edge to Edge repair (M-TEER)’ procedure.
What will happen to me before the procedure?
Before you have your Mitral TEER, your doctors will carry out a number of tests which will enable them to know more about your heart. As well as routine blood tests, you will have a transthoracic/ transoesophageal echocardiogram (ultrasound scan of your heart from the front of your chest/ through the foodpipe to assess your heart pump function and the severity of your Mitral valve disease). You may also require a magnetic resonance imaging (MRI) scan, a lung function test (to see how well your lungs are working), and an angiogram (when a catheter is placed into an artery in your leg and x-ray pictures are taken of your heart and arteries using special dye). We will explain any tests to you in full and you will of course have the opportunity to ask any questions. Following completion of tests, each case is discussed in our multidisciplinary meeting involving interventional cardiologists, cardiac surgeons and echocardiography consultants and appropriate candidates will be offered the procedure of Mitraclip.
What will happen to be on the day of the procedure?
A Mitral clip or TEER procedure requires a general anaesthetic. Anaesthetists are doctors who have had specialist training in anaesthesia, in the treatment of pain, in the care of very ill patients (intensive care), and in emergency care (resuscitation).
On the ward
An anaesthetist will visit you on the ward before the operation to discuss your anaesthetic. The anaesthetist needs to find out about your general health, previous experiences of anaesthesia, any medicines you are taking and any allergies you might have. If you have caps or crowns on your teeth, please tell the anaesthetist at this time, as these can occasionally be damaged during anaesthesia. This is a good time to talk about any previous experiences you have had with injections or hospitals, or any particular concerns you have. For practical reasons, the anaesthetist who comes to see you on the ward may not always be the same one who gives you the anaesthetic, but the information you give them will be passed on. Occasionally, your anaesthetist may find something about your general health that could increase the risks of your anaesthetic or operation. It might then be better to delay your operation until the problem has been reviewed. This could happen if you have a cold, rash or infection.
Eating and drinking
It is important that your stomach is as empty as possible before the anaesthetic. Usually, you must not eat anything at all for six hours before your procedure but you may drink clear fluids (e.g., water) up until 4 hours before your procedure. The nurse looking after you will tell you when you need to stop eating and drinking.
Before the procedure
The anaesthetist may prescribe a sedative (pre-medication) to be given by the nurses before you go for your procedure. Pre-medication or ‘pre-med’ is a medicine that is given to you to help you to relax. It will usually be given to you in the form of a tablet.
You will then be taken to the cardiac catheterisation lab. One of the nurses from the ward will come with you and stay with you until you are transferred into the care of the anaesthetist. When you arrive in the catheterisation lab, the anaesthetic assistant will check your details, and you will be transferred onto the operating table and moved into the anaesthetic room. Here, the anaesthetic assistant will attach you to a heart monitor and place a pulse and oxygen monitor on your finger.
The anaesthetist will then put a needle into a vein in your hand or arm, through which the anaesthetic can be given to send you to sleep. You may also be aware of him/her injecting some local anaesthetic into your wrist in order to place a small tube into an artery. You will also have two drips put in before you go to sleep – one in a vein in your arm, and one in an artery in your arm. These let us give you drugs and fluid before the procedure.
After this, you will receive some oxygen from a mask and the anaesthetist will start to give you the anaesthetic medication. Once you are asleep, a tube will be placed in your windpipe so that the anaesthetist can support your breathing during the procedure and further drips will be put in place: some into veins in your arms, and some into veins in your neck. A catheter may be put into your bladder to drain urine during the procedure. All of this allows us to monitor you closely during the operation and to give you drugs and fluid.
What will happen to be during the procedure?
Once you are asleep, we will also pass an ultrasound probe into your gullet (also known as your oesophagus or “food pipe”). This allows a doctor to use “transoesophageal echo” (TOE). A TOE is a special type of ultrasound that uses sound waves to take very clear pictures of the heart. This helps your doctor guide the catheters into place in your heart and to guide placement of the clip onto your Mitral valve.
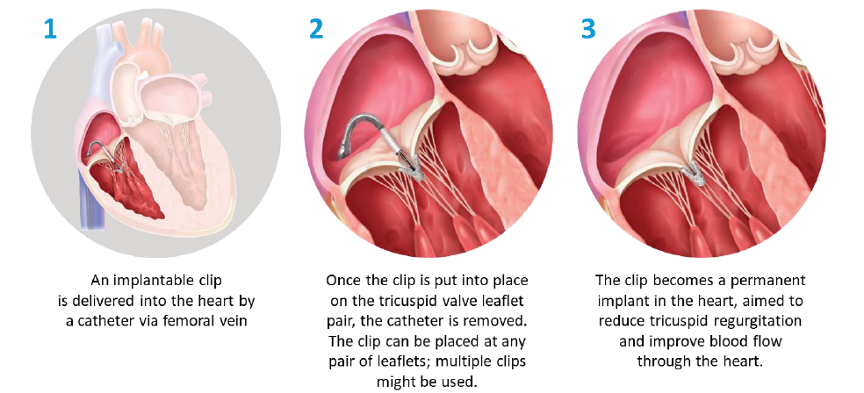
A small incision (cut) is then made in your groin through which your doctor will insert a small tube, followed by a catheter. Using x-ray pictures, the doctor will guide this catheter into your heart. Once this has been performed, we can deliver the Clip into position to repair the leak of the Mitral valve.
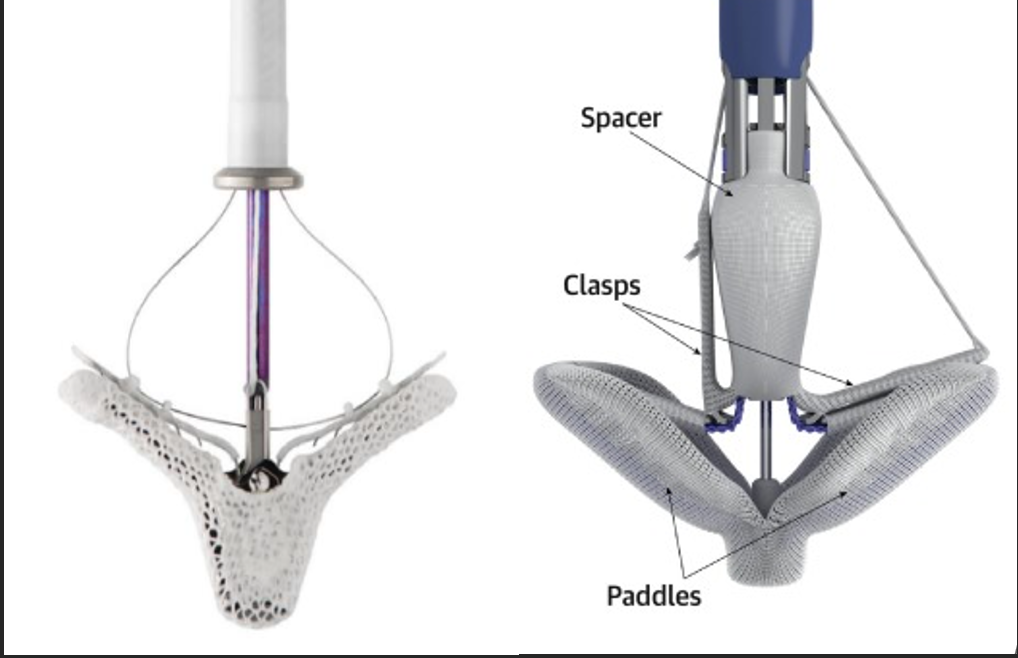
The Clip holds the two edges of the Mitral valve leaflets in position and reduces the extent of the leak. The end result is a Mitral valve with two or three openings instead of one with blood able to flow through the orifices forwards into the left ventricle.
What happens after the procedure?
After the procedure you will be taken to the intensive care unit or the recovery unit for observation. Once your condition is stable, you will be moved to a cardiology ward. As you recover you will be closely monitored. If you experience any pain this will be treated with pain-relieving drugs. You will have a repeat transthoracic echocardiogram the day after your procedure to assess the degree of any residual (left-over) Mitral regurgitation.
How long will I be in hospital?
Patients usually come to hospital the day before their Mitraclip to allow full preparation and complete any investigations required. We expect you to leave hospital between one and two days after the procedure.
What are the benefits of the procedure?
This procedure should reduce your Mitral regurgitation, so improving the symptoms of heart failure and reducing the fluid overload.
What are the risks?
No medical procedure is entirely without risk. It is important to remember, though, that your doctors would not have recommended having this procedure if they did not believe the potential risks were outweighed by the likely benefits to your health.
You are being considered for this treatment because you are felt to be at high risk for a serious complication during or following conventional surgical Mitral valve repair. We feel that a Mitraclip (trans-catheter valve repair) will carry fewer risks for you. However, there are still risks to consider and additional unknown side effects cannot be ruled out.
Important risks to you from this procedure include the following:
- Failure of the valve repair to work satisfactorily <2%
- Bleeding
- Abnormal heart rhythms
- Collection of blood around the heart requiring drainage using a needle or surgery
- Damage to the blood vessel requiring surgical repair
- Device embolization: the device moving out of position after implantation is rare but remains a possibility.
- Stroke <1%
What are the alternatives?
Mitral regurgitation is traditionally treated with open heart surgery to repair or replace the leaky Mitral valve. As you know, we think you are at high risk of conventional surgery and so are suggesting this alternative approach. The risks set out above need to be balanced against the risk of you not having the procedure and leaving the valve as it is now which means you would continue to experience the symptoms you have now such as fatigue, and fluid overload. If you do not want to have an operation, we can use medication to manage your symptoms but your underlying heart problem will continue to deteriorate. It is important to discuss the effects of not having the procedure with your doctor.
What medication will I need to take?
You will need to continue on most of your medication, including anticoagulation. If you are not already anticoagulated, you may need a short course of blood thinning tablets (such as Aspirin, Clopidogrel or Warfarin).
